Victoria Sevilla was a Virtual Global Health Practicum Intern for CFHI Philippines in February 2022. She was mentored by Associate Medical Director Paolo Victor Medina, MD. Victoria received her Bachelor’s in Global Health from the University of Southern California (USC), and will earn her second degree in Biological Sciences this year. She credits GlobeMed at USC for catalyzing her dedication to health equity and social justice, but the scope of her activism has since expanded. Victoria holds positions in Right to Health (R2H) Action, a grassroots health policy organization, and the American Medical Women’s Association (AMWA). She is also a member of the American Medical Student Association (AMSA) and the American Public Health Association (APHA).
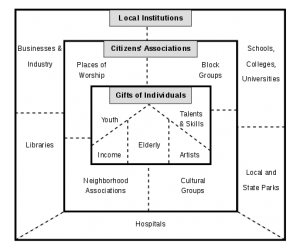
For years, I’ve longed to work with CFHI due to their sustainable model with fair-trade partnerships and asset-based community engagement. My undergraduate work with GlobeMed at USC emphasized the importance of responsible global health collaborations, especially avoiding volunteer tourism or “voluntourism.” Despite ramifications to the local communities, traveling to lower- or middle-income countries to “help the less fortunate” is a swiftly growing trend.
Having native Tagalog fluency, I knew my capacity to contribute a culturally-sensitive impact was expanded should I participate in CFHI’s Global Health in the Philippines program. I also understood, however, that my experiences greatly differed living in the United States. In addition to limited financial resources as a student, I did not feel qualified to travel to and volunteer in a country I had not visited since childhood. So upon learning of CFHI’s virtual programs, I was excited for the opportunity to broaden my global health competencies without infringing ethical dilemmas.
Voluntourism is not limited to eager tourists and also extends to the medical community. Historically, medicine has been used to biologically justify racial supremacy.1 As a result, colonizers excused medical research on native populations and the eradication of their history, culture, and language.1 Today, healthcare professionals could perpetuate this colonial legacy by performing medical procedures typically beyond their scope of practice.1 For pre-medical students, volunteering abroad is part of the “pre-med” checklist to look better on medical school applications, all while gaining clinical experience not otherwise allowed in the United States. These undergraduates, untrained and unqualified based on American standards, capitalize on the opportunity with minimal or no accountability.
Though “voluntourists” claim altruistic intentions, a “White Savior,” capitalist-colonial subjectivity remains.2 Voluntourism not only reinforces distorted power-dynamics between countries and disrupts local economies, it coerces those already resource-strained to adapt.4 Medically, cultural differences and language barriers severely compromise patient safety, especially in rural communities where access to care is scarce.1 Pre-health students are most dangerous, some having been allowed to diagnose patients, write prescriptions or perform medical procedures by themselves.3 And with more and more natural disasters and extreme weather, the demand for these “humanitarian expeditions” is predicted to increase.4 Another layer of complexity are the growing concerns about the misuse of technological advances where “virtual volunteerism” could become another mode of exploitation.4 For these reasons, voluntourism is really a form of neocolonialism.
So where does this leave global health students? How do we gain real-life experiences without partaking in the unethical practices we advocate against? We are not excused from “intellectual tourism” simply because of our academic status.5 Thus, Withers et al. (2018) and the Association of Pacific Rim Universities (APRU) identified the major obstacles faced in academic practicums and established best practices in response.5
Major Challenges:5
- Sending vs Host Institution Disputes
- Language and Cultural Differences
- Intentional or Accidental Misconduct
- Unequal Benefits from Partnership
- Inadequate Mentorship
- Student Financial Disparities
- Practicum Value
- Physical Safety
Best Practices Recommendations:5
- Competitive Student Selection
- Transparency on Objectives and Expectations
- “Pre-Trip” Orientation
- Pre‐requisite Training
- Financial Aid
- Mutual Benefit and Reciprocity
- Pertinent Mentorship
- Program Assessments
CFHI’s model ensures these challenges are addressed and best practices maximized. With the help of Dr. Juliana Araya Amador (CFHI Practicum Coordinator) and Dr. Paolo Victor Medina (CFHI Philippines Associate Medical Director and Practicum Preceptor), I was confident my actions were not only ethical and sustainable, but also exemplified the cultural humility CFHI values.
In addition to practicing and teaching Community Medicine as an Assistant Professor at the University of the Philippines College of Medicine, Dr. Medina is the faculty liaison officer to the town of Ternate under the MAGNAMARTE-UP Community Health Partnership Program. With guidance from Ternate’s Municipal Health Officer and based on the town’s current needs, Dr. Medina designed my project to study vaccine hesitancy. The practicum objectives, key responsibilities and expected deliverables were clearly communicated, and all of my questions immediately addressed. At the “pre-trip” orientation stage, online modules included analyses of my cultural profile and intercultural effectiveness, identifying the cultural differences I should be most attuned to. Most valuable of all is Dr. Medina’s impeccable mentorship. His patience and thorough guidance ensured my academic, professional, and personal development surpassed its potential.
Contributing to equitable healthcare delivery to vulnerable populations is an indescribable honor. Currently, there is minimal literature on Filipino COVID-19 vaccine hesitancy, and rural communities are especially at the margins. Working with the citizens of Ternate, we hear their causes for concern and factors in decision making. Promoting open discourse allows us to strategize the best, next steps forward with the local government. Though the 16-hour time difference minimizes direct resident interactions, Dr. Medina and I are able to use it to our advantage. Completing the investigative analysis in my time zone maximizes the field team’s reach in the community. We are literally working around the clock! This efficiency is made possible by the virtual platform and has promising applications for interdisciplinary collaborations.
As Dr. Mellissa Withers’s (APRU Global Health Director) former student, I have had the privilege of her instruction and guidance. Discussing virtual global health practicums and the applicability of APRU’s Best Practices, she supports the expanded accessibility for students. She does not believe it perpetuates neocolonial volunteerism because performative tourists driven by a savior mentality will prefer traveling in-person. Dr. Withers concludes that the ultimate gauge on responsible global health engagement depends on the hosts’ investment and if it strains their resources.
CFHI’s virtual programs allowed international partnerships to progress at a time where borders were closed, but global health collaboration even more dire. This innovative response to the pandemic demonstrates how ethical and sustainable practices can be maintained despite society’s thrust into survival mode.
Learning from esteemed leaders such as Dr. Medina, Dr. Withers, and Dr. Araya is an unbelievable privilege, and I am beyond grateful for the opportunity CFHI has enabled. This practicum experience is a comprehensive application of the competencies I’ve learned, and I hope to participate in an on-site rotation in the future. For students concerned with the wider implications of their global health involvement, CFHI’s well-established infrastructure is a testament to their mission towards responsible engagement.
References:
- Eichbaum, Q.G., Adams, L. V., Evert, J., Ho, M-J., Semali, I. A., & van Schalkwyk, S. C. (2020). Decolonizing Global Health Education: Rethinking Institutional Partnerships and Approaches. Academic Medicine, 96(3), 329–335. https://doi.org/10.1097/ACM.0000000000003473
- Everingham, P. & Motta, S. C. (2020). Decolonising the “autonomy of affect” in volunteer tourism encounters. Tourism Geographies, 1–21. https://doi.org/10.1080/14616688.2020.1713879
- Evert, J., Todd, T., & Zitek, P. (2015). Do you GASP? How pre-health students delivering babies in Africa is quickly becoming consequentially unacceptable. The Advisor, 61-65.
- Ong, F., Lockstone-Binney, L., King, B., & Smith, K. A. (2014). The Future of Volunteer Tourism in the Asia-Pacific Region: Alternative Prospects. Journal of Travel Research, 53(6), 680–692. https://doi.org/10.1177/0047287514532365
- Withers, M., Li, M., Manalo, G., So, S., Wipfli, H., Khoo, H. E., Wu, J. T., & Lin, H. H. (2018). Best Practices in Global Health Practicums: Recommendations from the Association of Pacific Rim Universities. Journal of Community Health, 43(3), 467–476. https://doi.org/10.1007/s10900-017-0439-z










 As a long time partner of the United Nations Economic and Social Council (UN ECOSOC), Child Family Health International (CFHI) had the honor of being invited to the
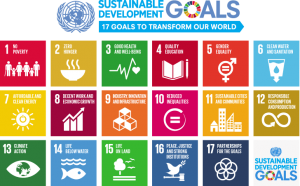
As a long time partner of the United Nations Economic and Social Council (UN ECOSOC), Child Family Health International (CFHI) had the honor of being invited to the  stressed in her keynote speech that, “we cannot achieve anything without partnership. It simply won’t happen.” In conversation amongst foreign diplomats and UN members, the importance of inclusive, bold and innovative partnerships was discussed in order to strive for resilient infrastructure and to honor the Sustainable Development Goals (SDGs), with special regard to vulnerable countries and a changing climate.
stressed in her keynote speech that, “we cannot achieve anything without partnership. It simply won’t happen.” In conversation amongst foreign diplomats and UN members, the importance of inclusive, bold and innovative partnerships was discussed in order to strive for resilient infrastructure and to honor the Sustainable Development Goals (SDGs), with special regard to vulnerable countries and a changing climate.